It is generally agreed that informed consent is a process whose effectiveness is a factor of a few core criteria. These criteria are typically held to include concepts such as disclosure, understanding, capacity, and voluntariness. Though guidelines differ somewhat in details or emphasis, they share a common thought: that through the informed consent process all relevant information about the study should be disclosed to the prospective participant; that the participant should adequately understand the information; and that the participant should have the capacity not only to comprehend the information, but also to knowingly and voluntarily agree to take part in the study, under the conditions disclosed to them.
But these criteria come with some challenges that can be thought of as deriving from different aspects of the nature of informed consent both as a concept and as a process. It is worthwhile, therefore, to briefly discuss that nature. i-CONSENT has explored some concepts to be taken into account and examined in greater depth.
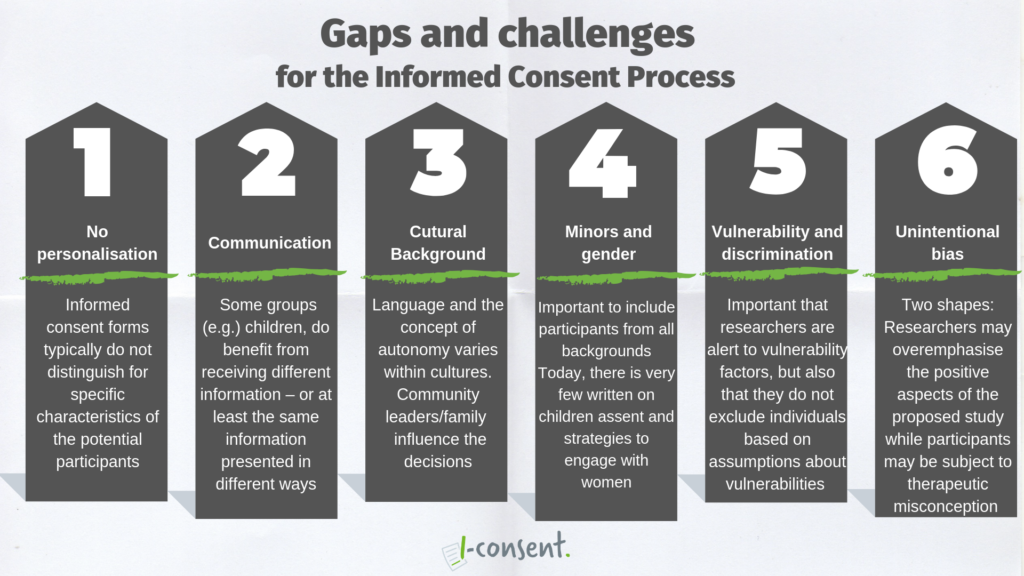
GAP 1. No personalisation
The inclusion in clinical research of people of all ages, genders, and backgrounds is extremely important. In order to successfully address the challenges to informed consent posed by promoting such inclusion, it is important to strive, as far as possible, to adopt individualised approaches, i.e. to focus on the particular circumstances and characteristics of individual prospective participants, rather than adopting standardised approaches or group-based approaches.
GAP 2. Communication
Another important question is, therefore, whether there should be different informed consent procedures for different groups, or, similarly, whether there should be room for variation in certain aspects of the process for different groups. This issue requires careful thought. On the face of it, it would seem, as a matter of fairness, that everybody should get the same information (at least on the paperwork). However, research reviewed in i-Consent Work Package 1 suggests that some groups do benefit from receiving different information – or at least from receiving the same information presented in quite different ways.
GAP 3. Cultural background
Variations in the way that participants assess the informed consent process are to be expected when we consider the diversity of cultural backgrounds. Many cultures approach the concept of autonomy differently to the most commonly approaches in European Union Member States (which is not to discount diversity of opinion within and between Member States). In some cultures, community leaders and/or family members can have a significant influence in determining whether a participant takes part in research. This is just one indication of the ways in which it can be challenging for researchers to identify culturally appropriate and respectful means to request informed consent. What works in one cultural setting cannot be uncritically assumed to work in another.
In line with this, the need to translate informed consent forms and other paperwork into participants’ languages is commonly cited as a problematic area. Effective translation requires cultural competence and thus it should not be assumed that a simple word-for-word translation will suffice. As mentioned above, the process of delivering information is context-dependent, norm-dependent, and it really matters how you say something. Translations that are not sensitive to background cultural contexts and norms are liable to misfire.
GAP 4. Minors and gender
It is important to include participants from all backgrounds not only as a matter of inclusivity, but as a matter of sound scientific method. In this regard, the involvement of minors in clinical trials has been a contested issue. Some studies have suggested that minors should only be included in clinical trials when it would be impossible to include adults instead – a view which seems rooted in the idea that minors are vulnerable and require protection.
As well as with regards to representation, being a minor means having a certain legal status: it says nothing of one’s maturity. This is where parenthal autority and childrend’s assent come into play, another challenge to the Informed Consent Process.
With regards to gender, i-CONSENT researchers found that while soft law resources often recommend and promote women’s participation in clinical trials – as participants, as researchers, as representatives of patient associations, and as members of ethics committees – specific strategies to achieve this are not provided. There is a gap here that must be bridged.
GAP 5. Vulnerability and discrimination
All guidelines advert to the need to identify and respond to vulnerability in prospective research participants. The question of vulnerability is a difficult one. People’s identities and circumstances are always multifaceted and any person can reveal vulnerabilities based on contextual parameters, situational factors and variables associated with procedural aspects of the research study. It is important that researchers are alert to these vulnerability factors, but also that they do not exclude individuals based on assumptions about vulnerabilities due to membership of a group or community.
GAP 6. Unintentional bias
Research in i-CONSENT suggests that, in addressing the challenges to informed consent, it is important to be aware of the role that biases – whether from psychological or cultural origins – play in influencing both participants and researchers. One manifestation of this can be bias in selection of participants by researchers who unintentionally favour prospective participants they find it easier to communicate with.
Here there is tension between, on the one hand, the importance of fostering trusting relationships between researchers and participants and, on the other hand, the importance of including less-well represented groups (e.g. from minority backgrounds) in studies.
A further form of bias is optimism bias. This can manifest in various ways affecting both participants and researchers. As regards researchers, they may have a tendency to overemphasise the positive aspects (potential benefits, for example) of the proposed study (the nudge); while participants may be subject to therapeutic misconception. Therapeutic misconception – the false supposition by a participant that their involvement in a trial is likely to have a positive therapeutic benefit – is a key concern that came up throughout all the i-CONSENT’s research including the consultations with patient groups.
This summary document shows that there are many challenges to the traditional informed consent process. Can we identify any common theme among them? Arguably we can. In the majority of cases, in order to properly ensure respect for a participant’s fundamental rights and interests, it is necessary to treat them as a unique individual, with a specific background and set of characteristics which make for an idiosyncratic array of vulnerabilities.
The use of digital technologies in the informed consent process seems to hold a lot of promise, even if the evidence of its effectiveness is currently somewhat mixed. The potential uses of these technologies is currently being researched in i-Consent Work Package 2.
Review the full text with the results of the investigation carried our in the frameworks of WP1 here.
